Before beginning any clinical activity, healthcare providers explain to a patient what they plan to do, what they hope it will accomplish, and any risks or side effects the patient may face. Then, the patient can agree to the plan or not. Without taking — and documenting — both of these steps, it’s unethical for a healthcare provider to proceed with treatment. It’s also legally hazardous.
This process of sharing information and obtaining permission is called informed consent. It’s the prevailing standard of care in all branches of medicine, and it’s a requirement in medical fields as disparate as research, device approval, clinical practice, and — our purpose here — mental health. Informed consent in psychology is the same as informed consent anywhere else in medicine in one important respect: It’s mandatory.
Psychology, mental health, and informed consent
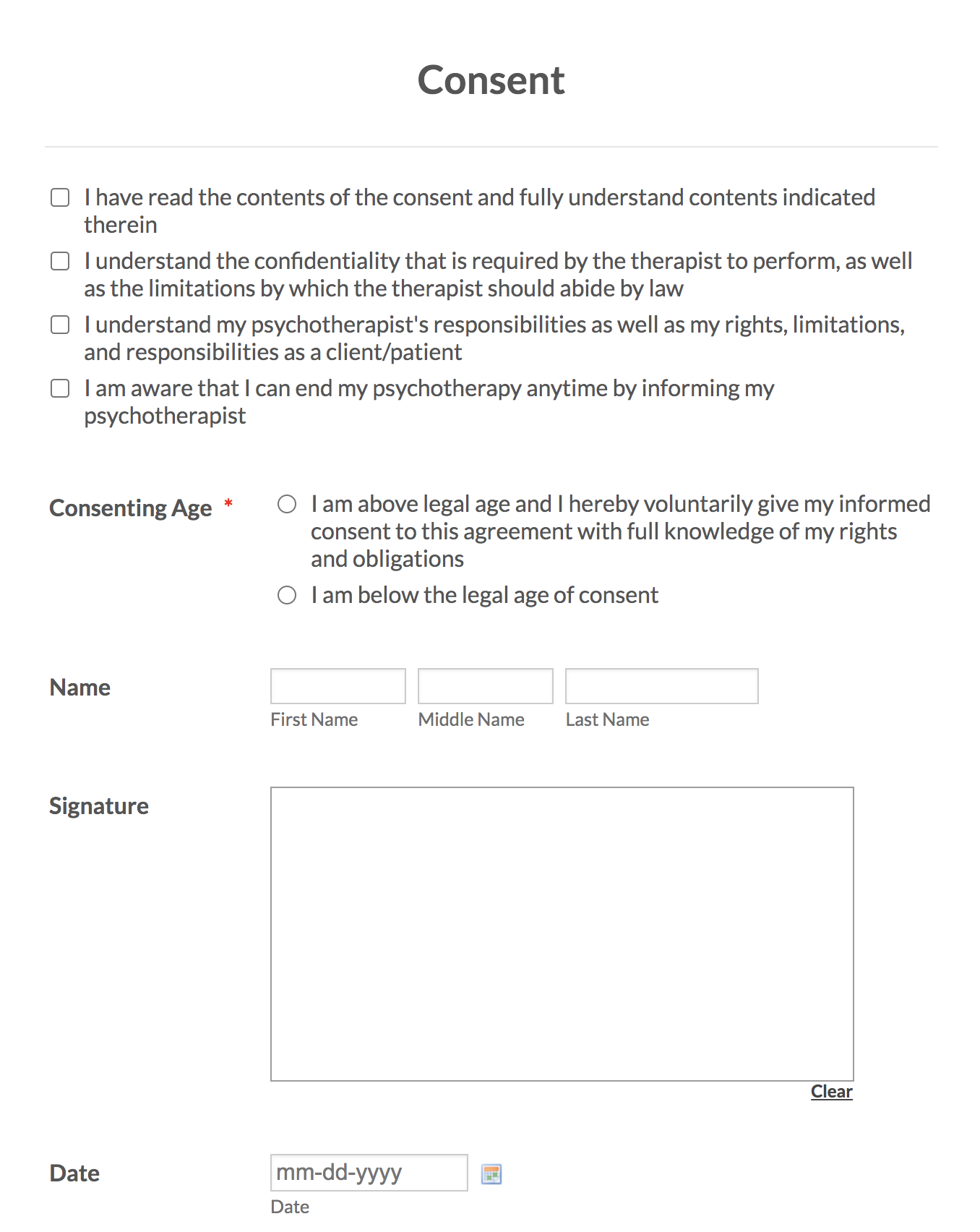
Psychologists aren’t the only mental health professionals who collect signed informed consent forms from their patients before beginning treatment. Therapists, clinical social workers, and counselors of all descriptions also make informed consent a regular part of their practices.
“Informed consent should cover everything regarding what the client can expect from treatment and how you run your therapy practice,” says Katie Ziskind, a licensed marriage and family therapist and owner of Wisdom Within Counseling. “Your client will sign legal documents that cover your practice and privacy policies, but they will also sign an informed consent form for psychotherapy before seeing you [the therapist].”
Informed consent is built into the ethical codes of professional associations, both local and national. The most influential of these is the Ethical Principles of Psychologists and Code of Conduct from the American Psychological Association (APA). Here’s what the APA has to say about informed consent in psychology.
Check it out…
Securely collect informed consent on any device with Jotform’s HIPAA-friendly online forms.
Informed consent in the American Psychological Association’s code of ethics
Section 3.10 of the APA’s Ethical Principles tells psychologists to obtain informed consent from patients before diagnosing or treating them. Later chapters describe the specific information psychologists should include on their consent documents. This differs by application. Informed consent forms for a psychological assessment, evaluation, or diagnosis should provide the following details, according to section 9.03 of the APA’s code of ethics:
- How and why the psychologist wants to assess, evaluate, or diagnose the patient
- The cost of treatment
- Any third parties that will participate in the assessment (testing labs, for instance)
- The patient’s confidentiality rights and the limits of those rights
- An offer to discuss the activity further prior to signing the form
An informed consent document for a patient preparing to enter therapy would include the last four items on that list, as well as details on “the nature and anticipated course of the therapy,” according to section 10.01 of the APA’s Ethical Principles.
Informed consent for a psychological research study is more involved. According to section 8.02 of the Ethical Principles, it requires researchers to explain
- What the research will entail and why the researcher(s) are conducting it
- The subject’s freedom to quit the study whenever they want
- What, if anything, will happen if they do quit the study
- Potential risks, negative side effects, and anything else that may make the subject want to quit the study
- The benefits of the research — to the subject and/or the science of psychology
- The subject’s rights to confidentiality and/or lack thereof
- How much, if any, the study pays
- Who to contact for answers to questions about any of the above
According to the Ethical Principles, when sharing information required for informed consent in any of these applications, psychologists should use simple, clear language that people without medical degrees can easily understand. Whether they share the key details verbally, electronically, or via spotty photocopy, psychologists must document the patient’s consent. The simplest way to do this is with an electronic signature.
But section 3.10 of the APA’s Ethical Principles also points to the changing nature of patient signatures. Psychologists can treat their patients in person or “via electronic transmission or other forms of communication,” the latest edition says. A traditional, in-person practice has a stack of clipboards ready to go, preloaded with informed consent pages ready for signatures. Telehealth providers need online forms, which Jotform offers.
Online informed consent forms from Jotform
Customizable forms from Jotform make informed consent documentation simple. Mental health professionals can choose the appropriate informed consent template, edit it to fit their practice, and start collecting consent in moments. Or they can start from scratch, using Jotform’s drag-and-drop Form Builder to create a polished, user-friendly, and HIPAA-friendly informed consent form — in psychology or any other medical field.













Send Comment:
2 Comments:
More than a year ago
It is important to monitor your health. And mental health also plays a big role. Especially if you are trying to build healthy, harmonious relationships. Dating Someone with Anxiety: What You Need to Know and Do So you can understand yourself, as well as help your partner, if the need arises.
More than a year ago
nice