When the COVID-19 pandemic struck, healthcare providers had to find a way to deliver care to their patients. Telehealth proved to be a great way to triage and, in some cases, diagnose issues from afar. The U.S. Department of Health and Human Services (HHS) recognized the importance of telehealth and issued a waiver in March 2020 to allow Medicare to reimburse for more than 80 additional services.
Just so you know
You’ve got your medical toolkit ready to help those in need — but what about your telemedicine toolkit? With Jotform’s HIPAA-friendly telehealth platform, you can easily create online medical forms that keep sensitive health data safe.
Many healthcare providers shifted to telehealth quickly to meet the growing demand. Some of the procedures and tools may have been hastily cobbled together, as those new to providing virtual services had very little time to figure out how telehealth fits into the bigger picture of their practices.
However, now that some time has passed, and it seems telehealth is here to stay, it’s a good idea to reevaluate what you’ve put in place and align your tools and policies with telehealth best practices. Here are a few pointers to help you get started.
Start with an implementation team
While you’ve likely got some experience delivering telehealth services, you should take a look at what you’re doing right now and what you can do better. If you’re part of a larger organization, it makes sense to assemble an internal team of staff and physicians.
This team can gather feedback and provide input on what’s been working and what hasn’t. For example, the IT staff member might note that it’s been difficult to support remote access for the electronic health record (EHR) software, so it may be necessary to consider an upgrade.
Set goals for the telehealth program
At first, rolling out telehealth was about providing patients with care since they couldn’t be seen in the office. Now it’s time to set clear goals for a more permanent program as part of your telehealth best practices.
One of the overarching goals could be to expand access to patient care, which is especially important in areas with underserved populations. This could also be useful in caring for geriatric patients and patients with chronic conditions who will have trouble traveling to the office for routine appointments.
Use appropriate technology
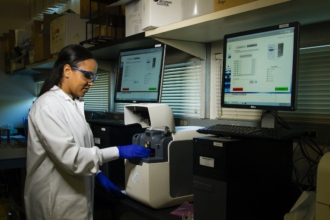
There are a lot of technology tools available for telehealth. While the most widely used one during the COVID-19 pandemic was video conferencing, telehealth also includes remote patient monitoring, technology to transmit radiology images, and more.
Depending on what you plan to do, you’ll need to evaluate the different types of tools available. Make sure they offer the Health Insurance Portability and Accountability Act (HIPAA) options to protect your patients’ information.
Have a backup plan
While technology today is pretty solid, there’s always a chance it won’t work. Your internet connection could go out, or your patients’ data could be lost if your cloud storage provider isn’t secure. Take into account all sorts of technology scenarios and plan for them appropriately.
For example, if you lose power in your location, you won’t be able to conduct telemedicine sessions from a computer because your router will probably be offline. You should know what kind of backup you have — like an emergency power supply or a mobile device that will let you connect.
Educate patients and staff
Unfortunately, people can be the weakest link in a plan even if you have the strongest strategies in place. When it comes to education, too much is never enough, especially when you’re handling patient data. Teach your staff telehealth best practices for patient data collection and storage — as well as HIPAA-friendly practices when they have to share that information with other providers.
Your patients will also need to learn how to use the telehealth technology you roll out, particularly if you send them home with remote monitoring systems. For example, they’ll need to know how to adjust their blood pressure cuffs or use their blood sugar monitors and upload the data to your EHR.
Obtain patient consent
Getting a patient’s consent to receive telehealth services is a critical best practice. Plenty of patients are new to this, and they may not know what to expect. Check your state and payer requirements to determine what type of consent you’ll need to get from the patient.
It’s wise to obtain written consent before a telehealth visit so that you have irrefutable proof that you provided the patient with their rights regarding treatment. You can do this by creating a form for them to fill out online before their appointment.
There are a lot of other telehealth best practices out there. As the use of virtual care expands, it’s important to stay on top of them to make sure that you’re not only providing the best possible care for your patients but also taking steps to protect their personal health information.















































Send Comment: