When COVID-19 forced cities into hasty lockdowns, many healthcare providers struggled with the overnight switch from onsite to digital services. “That weekend was hell for a lot of people,” recalls Dr. Marlene Maheu, founder and executive director of the Telebehavioral Health Institute.
Most psychologists had to quickly put together makeshift telepsychology services, without necessarily having the right documentation or workflow. Now, psychologists are facing the challenges of making sure their telehealth services comply with regulations and providing the level of service patients deserve.
The American Psychological Association (APA) has published specific telepsychology guidelines that every practitioner should be aware of, says Maheu. She strongly recommends going through the APA ethics code line by line to ensure you know how to satisfy all the requirements through telehealth. If your telepsychology service isn’t fulfilling the demands of each section, “remediation is in order,” Maheu says.
Below are four areas where many practitioners are falling short and some suggestions on how you can take action.
1. Be proactive about data security
In response to the COVID-19 emergency, the Office for Civil Rights relaxed its enforcement of Health Insurance Portability and Accountability Act (HIPAA) regulations for telehealth services. However, contrary to what some practitioners think, this doesn’t mean HIPAA is no longer necessary. Hackers have been exploiting patients’ increased use of online technology without sufficient security to steal sensitive information.
To be HIPAA-friendly, you must have a business associate agreement (BAA) — a formal agreement to maintain the security and privacy of patient data — with each software service you use.
Maheu advises practitioners to get educated on cybersecurity and do due diligence on the systems they plan to use. Most software isn’t built specifically for psychology services. As a practitioner, it’s your responsibility to apply any additional measures you need to meet your legal obligations for patient confidentiality.
“You have to understand the law and then pick your technology,” Maheu says. “Don’t pick your technology and then retrofit your services to match what the tech will let you do.”
2. Assess whether telepsychology is right for each patient
Establish a screening process to see if telepsychology is a good fit for each patient. “They may not have the technology or the bandwidth, or the finger dexterity and hand-eye motor control to work a mouse,” Maheu explains.
You may be able to resolve some of your patients’ challenges. If they don’t have access to a computer, could you offer services to them via telephone? If they don’t feel confident using videoconferencing software, can you arrange for a trusted family member to help set them up for their session?
An initial screening lets you identify who could benefit from telepsychology with extra support and who needs in-person services.
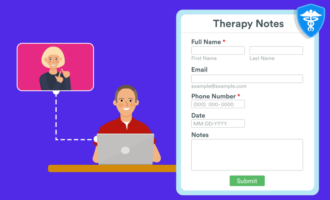
3. Obtain informed consent
The APA advises practitioners to obtain informed consent specific to telepsychology services. This includes explaining to patients how they will receive treatment and how their data will be stored.
If you’re building your informed consent document online, Jotform’s HIPAA-friendly online consent form template is fully customizable.
Many of the major professional associations for psychologists have sample informed consent documents to use as the basis for your own, but Maheu recommends that every practitioner write their own informed consent document.
“Nobody can make an informed consent document for you,” Maheu says, “because it is your duty to have that document reflect your state law and your ethical requirements for telehealth related to your profession. Get trained and learn to adapt your informed consent procedures as well as the document itself.”
4. Practice your emergency response
Telehealth poses particular challenges for emergencies. There can be additional risks when patients receive treatment at home, and it can be harder to control a situation if you’re not there in person. What if a patient shows up intoxicated or has a medical emergency while they’re on a video call?
Put together telehealth-specific emergency protocols and practice your response to clinical emergencies. If you don’t handle the situation in a professional way, you could discourage the patient from getting further psychological help. In a worst-case scenario, inadequate emergency response can seriously endanger their well-being or even their life.
The future of telepsychology
Telehealth services are here to stay, so it’s worth investing the time to manage telepsychology properly. “My prediction is that many practitioners will opt for a hybrid model,” Maheu says, with a combination of in-person and virtual healthcare.
Telepsychology greatly improves access to mental health support — patients don’t have to travel to see a specialist or regularly take time off work. But to be effective, telepsychology practitioners need to comply with all the applicable laws and offer a high level of service.
“We need to be professional in everything we do,” Maheu says, “so people don’t stop trying to get the help they need because their online experiences showed them that psychotherapy ‘doesn’t work.’ ”















































Send Comment: