3 different levels of oversight and auditing
Of all the subindustries of healthcare, the hospice field requires some of the most sensitive, nuanced conversations and care strategies. Terminally ill and end-of-life patients, as well as their friends and families, expect a high level of professionalism and quality from hospice care, so that they can find comfort and peace during a very difficult time.
Interdisciplinary groups, or IDGs, are at the center of hospice care for each patient, handling all aspects of care, from medication plans to bereavement counseling and everything in between.
Since IDGs are responsible for such sensitive care, they must ensure they conduct and document meetings and carry out all necessary tasks as effectively and transparently as possible. That means it’s imperative to maintain accurate hospice IDG documentation.
To illustrate the importance of hospice IDG documentation, here’s a breakdown of the three key hospice auditors and their processes, how hospice organizations can properly prepare, and some ways that digitization can make documentation even easier.
Understanding hospice IDG documentation auditing
Depending on the type of facility, there are three different levels of oversight and auditing for hospices: federal, state, and third-party. These entities ensure that hospice care meets every required standard, including HIPAA.
1. Federal hospice regulators
The highest level of hospice auditing authority, federal regulators predominantly review whether hospice IDG documentation complies with national standards laid out by Medicare and other regulatory bodies. These federal investigations take two forms.
The first is a Targeted Probe and Educate (TPE) audit conducted by Medicare administrative contractors (MACs). These audits identify error-prone providers whose documentation processes — especially for claim filing and billing — pose risks to Medicare as a whole. MACs also work to provide an action plan for these organizations to fix flawed processes.
Other federal auditors include unified program integrity contractors (UPICs). Compared to MACs, these contractors focus less on solving system-wide issues and more on rooting out bad actors, aiming to eliminate fraud, abuse, and waste within the federal hospice system.
2. State hospice regulators
At the next level of hospice regulation, state departments of health (including comptrollers and local healthcare agencies) conduct regular audits. In reviewing documentation, these state-level auditors ensure compliance with state healthcare policies as well as assist investigations at the federal and private levels.
3. Third-party hospice regulators
The third rung of hospice regulation deals with for-profit and third-party hospice facilities. Other third-party individuals and regulators (like auditing and law firms, for example) or the aforementioned national and state auditors can conduct audits of these facilities.
Historically, private hospice facilities are just as susceptible to fraud, waste, and abuse investigations, highlighting the need for accurate hospice IDG documentation. California, the state with the most for-profit hospice programs, has seen abnormally high patient discharge rates, likely due to improper documentation of patient information and need.
Ensuring hospice IDG documentation quality
Proper hospice IDG documentation is essential to providing necessary patient care and keeping the family members and friends involved well informed. Documentation should be clear and offer actionable takeaways that make sure patients receive high-quality and accurately funded treatment (and that hospice facilities avoid overspending or misspending funds).
IDGs must ensure documentation is always complete and accurate, and that it displays a clear terminal progression with regular updates on the patient’s illness or health status. More specifically, documentation language should provide detailed metrics of progression instead of vague indications of general decline (which often lead to investigations of fraud).
To maintain consistency and protect the integrity of Medicare funding, there should be a full record of previous treatment facilities (hospice facilities especially) that have been involved in the patient’s care.
In addition to this documentation to-do list, organizations need to make sure their method of collecting, storing, and distributing all patient information is HIPAA-friendly to avoid breaches of trust or costly fines.
Leveraging Jotform for hospice IDG documentation
An immediate way for organizations to improve their hospice IDG documentation is by digitizing it. A platform like online form builder Jotform can take the guesswork out of the security and accuracy worries related to hospice documentation, providing easily customizable and distributable forms for all IDG functions.
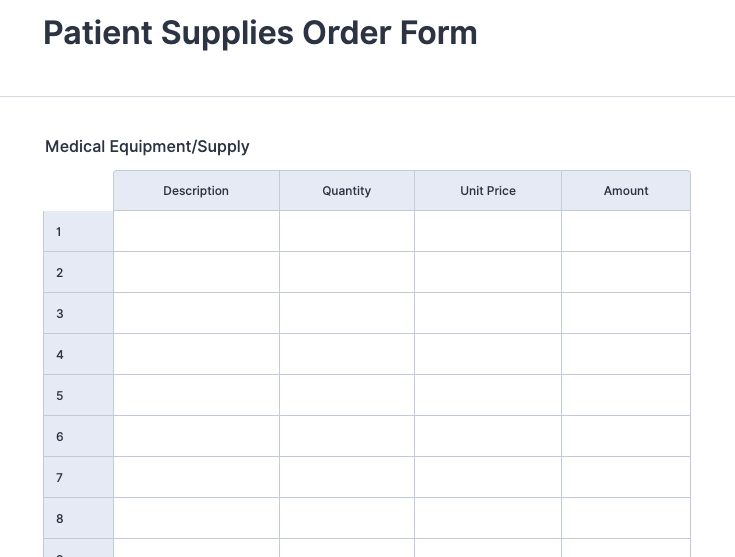
Jotform offers prebuilt HIPAA-friendly templates — including forms and tables you can use to easily manage, organize, and store documents — to guarantee your organization is protecting patient data.
Providing effective and efficient hospice care is challenging enough as it is without bureaucratic agencies getting involved. But maintaining accurate hospice IDG documentation isn’t just about avoiding fines and sticking to the rules — these records help assure that IDGs run to the best of their ability and each patient receives the best quality treatment.
With the right digital tools and comprehensive knowledge of regulations, hospice organizations can make sure patients and their loved ones feel that someone is taking good care of them.


















Send Comment: